Colorado Pediatricians Integrate Oral Health into Medical Checkups for Low-Income Families
Pediatricians integrate oral health into medical checkups, providing fluoride and referrals for low-income children lacking access to dental care.

Integrating Oral Health into Medical Checkups
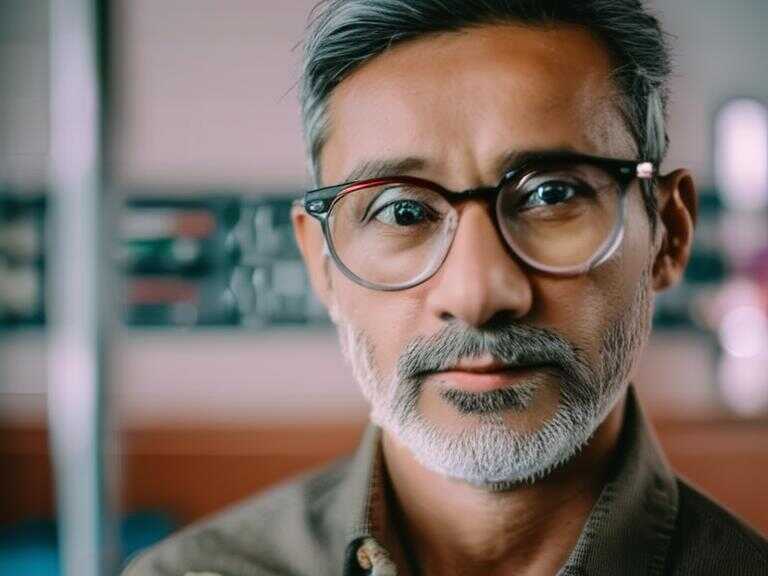
On a recent Monday, pediatrician Patricia Braun and her team attended to approximately 100 children at a community health clinic in Denver. Along with providing flu shots and treating illnesses like ear infections, Braun also incorporated oral health assessments into the medical checkups. She emphasized the prevalence of oral diseases within the population she treats at Bernard F. Gipson Eastside Family Health Center, which forms part of Denver Health, the largest safety-net hospital in Colorado, catering to low-income, uninsured, and underinsured residents. Braun’s efforts reflect a growing trend across the United States to integrate oral health into medical checkups for children, pregnant women, and individuals who face challenges in accessing dental care.
Expanding Programs and Overcoming Barriers
Over the past decade, federal and private funding has supported the expansion of programs aimed at integrating oral health into medical care. Despite this progress, these initiatives encounter socioeconomic barriers, workforce shortages, and the complexities associated with meeting the needs of new immigrants. In response to these challenges, Braun and her colleagues have utilized a five-year, $6 million federal grant to train 250 primary care providers in oral health across Colorado, Montana, Wyoming, and Arizona. Similar projects have been underway in Illinois, Michigan, Virginia, and New York, bolstered by funding from the federal Health Resources and Services Administration's Maternal and Child Health Bureau.
"We're taking that next step where care is not just co-located, meaning, say, we're upstairs and dental is downstairs, but we're integrated so that it becomes part of the same visit for the patient."
Pediatrician Patricia Braun highlighted the integrated approach adopted by their practice, emphasizing the seamless incorporation of oral health into medical visits. This approach involves the assessment, education, and provision of preventive care, with the added capability to refer patients to on- or off-site dentists, or collaborate with embedded dental hygienists as part of the healthcare practice. Tara Callaghan, director of operations for the Montana Primary Care Association, underscored the critical nature of providing these services during medical visits, citing its role in increasing the frequency of fluoride application and enhancing parents' knowledge of caring for their children's teeth.
Addressing Access Challenges
However, various obstacles hinder the effective delivery of integrated oral health services. Callaghan highlighted the difficulty in recruiting dental professionals in Montana, attributing it to the state’s large geographic area and small population. Additionally, she noted that fifty of the state's 56 counties are designated as dental shortage areas, further exacerbating the challenge of accessing dental care. Furthermore, the scarcity of pediatric dental specialists in rural areas often leads to families having to travel long distances to neighboring counties for care.
"State regulations vary on which services hygienists can provide without supervision from a dentist. In Colorado, Cuzella can, among other things, independently perform X-rays and apply silver diamine fluoride, a tool to harden teeth and slow decay."
Valerie Cuzella, a registered dental hygienist who collaborates closely with Braun and others at Denver Health, operates within the framework of state regulations, with the ability to perform certain tasks independently, such as X-rays and the application of silver diamine fluoride to fortify teeth and mitigate decay. This cooperation and delegation of responsibilities between medical and dental professionals signify a departure from the traditional siloed approach to healthcare.
Integration Efforts and Impact
Katy Battani, a registered dental hygienist and assistant professor at Georgetown University, has been involved in initiatives to integrate dental care into prenatal visits for pregnant women across nine states, including California, Texas, and Maryland. Battani emphasized the potential to leverage the frequency of medical visits during pregnancy to enhance oral health, particularly for women gaining dental coverage through Medicaid and receiving regular medical care. Sung Cho, a dentist overseeing the dental program at STRIDE Community Health Center in Denver, highlighted the inaccessibility of dental care for many children, the migrant community, and seniors due to various factors such as housing instability, language barriers, lack of transportation, and the high cost of dentistry without insurance.
Overcoming Financial Uncertainty
In the face of growing needs, Sung Cho expressed concerns regarding the financial uncertainty stemming from the Medicaid "unwinding" process. This process involves the reassessment of post-pandemic eligibility for the government program that provides health coverage for individuals with low incomes and disabilities. Cho highlighted the challenges in meeting the upfront costs of new staff and replacing aging dental equipment, underscoring the financial strain on healthcare providers seeking to meet the demands of their patients. Despite the challenges, there have been efforts to address workforce shortages in Colorado through the enactment of a law allowing dental therapists to practice, although the state faces the absence of schools to train or accredit them.
Impact on Preventive Oral Health Care
As a result of efforts to integrate oral health into medical care, providers in the Rocky Mountain region have administered over 17,000 fluoride varnishes and significantly increased the percentage of children aged 3 and younger receiving preventive oral health care, from 33% to 78% within the first 2½ years. Tara Callaghan of the Montana Primary Care Association emphasized the significance of leveraging the frequency of well-child visits to address oral health needs, particularly for at-risk children. These integrated approaches have yielded tangible improvements in preventive oral health care for vulnerable populations.
KFF Health News is committed to providing comprehensive coverage of health issues and operates as a core program at KFF, serving as an independent source for health policy research, polling, and journalism.
Share news